Please be advised we are currently operating at limited capacity, with some delays. Click here to contact us.
Detailed Test Information
The ability to digest and selectively absorb nutrients from our foods and beverages is one of the cornerstones of good health. To obtain benefits from food that is consumed, nutrients must be appropriately digested and then efficiently absorbed into portal circulation. Microbes, larger sized particles of fibre, and undigested foodstuffs should remain within the intestinal lumen. Poor digestion and malabsorption of vital nutrients can contribute to problems with degenerative diseases, compromised immune status, and deficiency states caused by inadequate mineral, vitamin, carbohydrate, fats, and amino acids status.
In addition to digestion and selective absorption, the gastrointestinal tract eliminates undigested food residues and toxins that are excreted via the bile into the intestinal tract and provides a niche for the proliferation of friendly microorganisms.
Impairment of the selective absorptive capacity or of the barrier function of gut (as in “excessive intestinal permeability”) can result from a number of suspected causes. Common associated causes include: low stomach acid; chronic maldigestion; food allergens’ impacting on the bowel absorptive surfaces; bacterial overgrowth or imbalances (dysbiosis); pathogenic bacteria, yeast or parasites with related toxic irritants; and the use of NSAID’s and antibiotics.
Impairment in intestinal function can contribute to the development of food allergies, systemic illnesses, autoimmune disease, and toxic overload from substances which are usually kept in the confines of the bowel for elimination.
Gastrointestinal (GI) complaints are among the most common reasons that patients seek medical care.
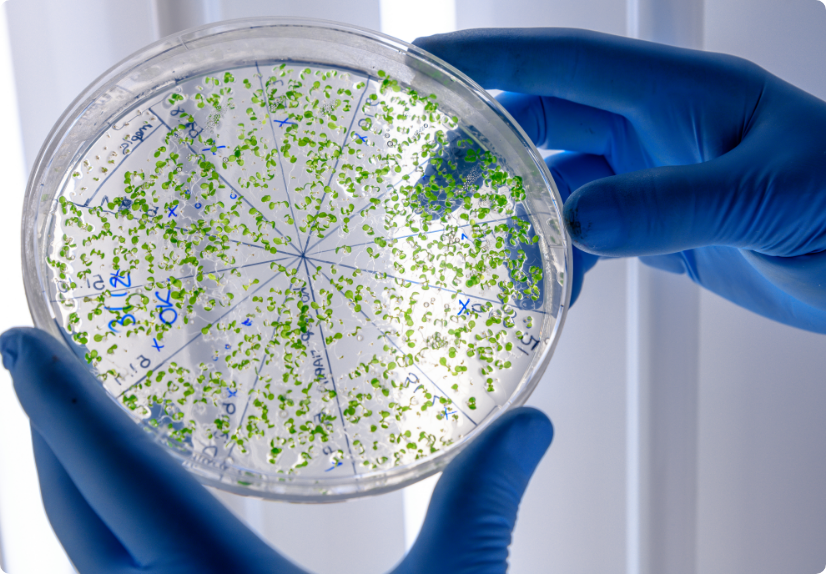
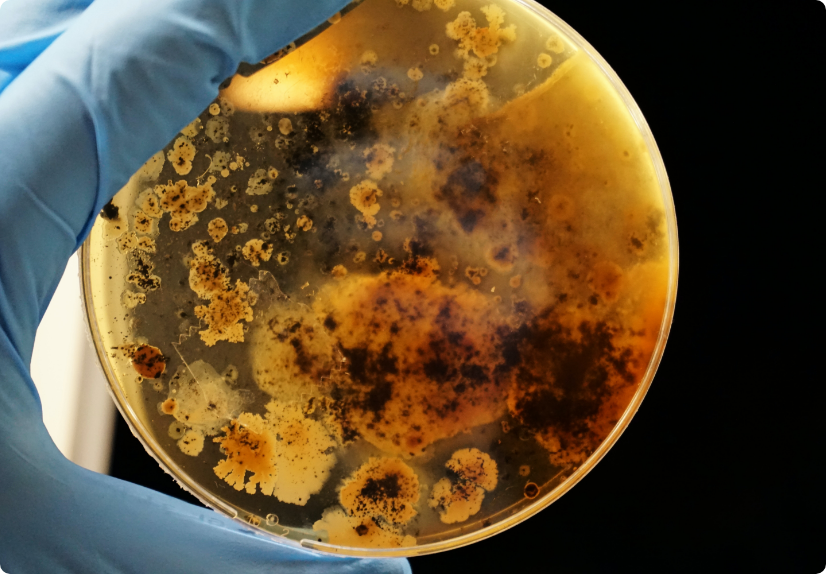
The Comprehensive Stool Analysis with Parasitology identifies live bacteria and yeast, parasites, maldigestion, bacterial metabolism, inflammation and immune function. Important information regarding the efficiency of digestion and absorption can be gleaned from the measurement of the faecal levels of elastase (pancreatic exocrine sufficiency), muscle and vegetable fibers, carbohydrates, and total fat.

A state where the beneficial host bacteria is compromised by an overgrowth of pathogenic bacteria. Pathogens can interfere with certain metabolic pathways and cause a knock on effect on other organ systems in the body. It is particularly beneficial to identify these pathogens to tailor a treatment plan accordingly and far more specifically.
Infection with yeast species can cause a variety of symptoms, both intra- and extra- gastrointestinal, and may escape suspicion as a pathogenic agent in many cases. Controversy remains as to the relationship between Candida infection and episodes of recurrent diarrhoea.

It is very important, and most cost effective, that 3 specimens are collected on 3 separate days. Parasites do not shed and their eggs do not appear on stool specimens on a homogenous/
regular basis. One day’s sample may produce negative results, while the following day’s sample may be positive.
Important information regarding the efficiency of digestion and absorption can be gleaned from the measurement of the faecal levels of elastase (pancreatic exocrine sufficiency), muscle and vegetable fibres, carbohydrates, and total fatty acids.

Elastase
the level of faecal Elastase is a useful measure of proteolytic activity and is closely correlated with protein digestion in the stomach, duodenum and small intestine. Decreased faecal Elastase values may reflect pancreatic insufficiency or decreased hydrochloric acid output within the stomach. Elevated faecal Elastase values suggest ingested food is travelling too quickly through the intestinal tract and is often associated with diarrhoea or rapid transit times.
Triglycerides
the fats and oils in our diets are mostly consumed as triglycerides — three fatty acids bound to one glycerol backbone. An elevated level of triglycerides in the stool indicates reduced fat hydrolysis by pancreatic lipase and is suggestive of pancreatic insufficiency.
Muscle fibers
the detection of muscle fibers in the stool indicates incomplete protein digestion. A variety of studies have shown a correlation between the presence of excessive faecal muscle/meat fibers and a reduction (hypochlohydria) or absence (achlorhydria) of hydrochloric acid secretion within the stomach and/or insufficient output of pancreatic enzymes (or excessive meat consumption).
Vegetable Fibers
the presence of excessive amounts of vegetable fibers is indicative of some type of maldigestion. An important factor to consider is that digestion starts in the mouth and the presence of significant amounts of vegetable fibers, especially if the vegetable is easily identifiable, suggests inadequate chewing or fast eating “on the run” may be contributing to maldigestion.

Inflammation can significantly increase intestinal permeability and compromise assimilation of nutrients. The extent of inflammation, whether caused by pathogens or inflammatory bowel disease (IBD), can be assessed and monitored by examination of the levels of biomarkers such as lysozyme, lactoferrin, white blood cells and mucus. These markers can be used to differentiate between inflammation associated with potentially life threatening inflammatory bowel disease (IBD), which requires life long treatment, and less severe inflammation that can be associated with the presence of enteroinvasive pathogens. Lactoferrin is only markedly elevated prior to and during the active phases of IBD, but not with IBS. Monitoring faecal lactoferrin levels in patients with IBD can therefore facilitate timely treatment of IBD, and the test can be ordered separately.
sIgA is the only bona fide marker of humoral immune status in the GI tract and represents the first line of defence of the GI mucosa by acting as the immune barrier. Since the vast majority of secretory IgA (sIgA) is normally present in the GI tract where it prevents binding of pathogens and antigens to the mucosal membrane, it is essential to know the status of sIgA in the gut. Elevated faecal sIgA levels generally indicate a response to antigenic presence.

Short Chain Fatty Acids are the end product of the bacterial fermentation process of dietary fibre.
The SCFA markers tested in the CSA give an indication of the individuals’ fibre intake as well as any potential dysbiosis that together determines the health of the intestinal tract. SCFAs decrease the pH of the intestines and therefore make the environment unsuitable for pathogens, including bacteria and yeast.
To ensure optimal levels, adequate fibre should be an important part of the diet. Sources of soluble fibre include fruits, vegetables, oat bran, barley, seed husks, flaxseed, psyllium, dried beans, lentils, peas. Sources of insoluble fibre include wheat bran, corn bran, rice bran, the skins of fruits and vegetables, nuts, seeds, dried beans and wholegrain foods; resistant starch include unprocessed cereals and grains, firm bananas, potatoes and lentils.
The role of SCFA’s includes their role as nutrients for the colonic epithelium, as modulators of colonic and intracellular pH, cell volume and other functions associated with ion transport, and as regulators or proliferation, differentiation and gene expression (Cook and Sellin, 1998).
The presence of Red Blood Cells or occult blood in the stool is a useful intestinal marker that provides insight in to whether there are any sinister conditions to further investigate. Its overall purpose is to tell us the health of the intestinal tract and in turn tailor treatment to the individual.
Normal healthy stool should be brown and soft but formed in consistency. Food and water consumption causes variations to the colour and consistency of the stool on a day-to-day basis. It is affected by pigments in foods, dietary supplements, bile, fibre, water and intestinal transit time. Keeping a check on the appearance of stool is an important way of ensuring the gastrointestinal tract is as healthy as possible to avoid chronic conditions developing.
Impairment of intestinal functions can contribute to the development of food allergies, systemic illnesses, autoimmune disease, and toxic overload from substances that are usually kept in the confines of the bowel for elimination. Efficient remediation of GI dysfunctions incorporates a comprehensive guided approach that should include consideration of elimination of pathogens and exposure to irritants, supplementation of hydrochloric acid, pancreatic enzymes and pre- and probiotics, and repair of the mucosal barrier.
Bacterial overgrowth/ Parasites/ Yeast
Intestinal Permeability
Decreased nutrient status, Compromised
Immune System, Low grade inflammation
Chronic degenerative Diseases
(Food allergies, Systemic illnesses, Autoimmune
disease, Toxic overload)
This analysis of the stool specimen provides fundamental information about the overall gastrointestinal health of the patient. When abnormal microflora or significant aberrations in intestinal health markers are detected, specific interpretive paragraphs are presented.
If no significant abnormalities are found, interpretive paragraphs are not presented.
Beneficial flora include lactobacilli, bifidobacteria, clostridia, Bacteroides fragilis group, enterococci, and some strains of Escherichia coli. The beneficial flora have many health-protecting effects in the gut, and as a consequence, are crucial to the health of the whole organism. Some of the roles of the beneficial flora include digestion of proteins and carbohydrates, manufacture of vitamins and essential fatty acids, increase in the number of immune system cells, break down of bacterial toxins and the conversion of flavinoids into anti-tumour and anti-inflammatory factors. Lactobacilli, bifidobacteria, clostridia, and enterococci secrete lactic acid as well as other acids including acetate, propionate, butyrate, and valerate. This secretion causes a subsequent decrease in intestinal pH, which is crucial in preventing an enteric proliferation of microbial pathogens, including bacteria and yeast. Many GI pathogens thrive in alkaline environments. Lactobacilli also secrete the anti fungal and antimicrobial agents lactocidin, lactobacillin, acidolin, and hydrogen peroxide. The beneficial flora of the GI have thus been found useful in the inhibition of microbial pathogens, prevention and treatment of antibiotic associated diarrhoea, prevention of traveler’s diarrhoea, enhancement of immune function, and inhibition of the proliferation of yeast.
In a healthy balanced state of intestinal flora, the beneficial flora make up a significant proportion of the total microflora. Healthy levels of each of the beneficial bacteria are indicated by either a 3+ or 4+ (0 to 4 scale). However, some individuals have low levels of beneficial bacteria and an overgrowth of nonbeneficial (imbalances) or even pathogenic microorganisms (dysbiosis). Often attributed to the use of antibiotics, individuals with low beneficial bacteria may present with chronic symptoms such as irregular transit time, irritable bowel syndrome, bloating, gas, chronic fatigue, headaches, autoimmune diseases (e.g., rheumatoid arthritis), and sensitivities to a variety of foods.
Treatment may include the use of probiotic supplements containing various strains of lactobacilli, bifidobacteria and enterococci and consumption of cultured or fermented foods including yogurt, kefir, miso, tempeh and tamari sauce.
Polyphenols in green and ginseng tea have been found to increase the numbers of beneficial bacteria. If dysbiosis is present, treatment may also include the removal of pathogenic bacteria, yeast, or parasites.
Certain dysbiotic bacteria may appear under the Commensal category if found at low levels because they are not likely pathogenic at the levels detected. These are more a sign of imbalances in other populations or elsewhere in the digestive tract. When imbalanced flora appear, it is not uncommon to find inadequate levels of one or more of the beneficial bacteria and/or a faecal pH which is more towards the alkaline end of the reference range (6.5 – 7.2). It is also not uncommon to find hemolytic or mucoid E. coli with a concomitant deficiency of beneficial E. coli and alkaline pH, secondary to a mutation of beneficial E. coli in alkaline conditions (DDI observations). Treatment with antimicrobial agents is unnecessary unless bacteria appear under the dysbiotic category. Addressing Concomitant imbalances remains the priority.
The microscopic finding of yeast in the stool is helpful in identifying whether the proliferation of fungi, such as Candida albicans, is present. Yeast is normally found in very small amounts in a healthy intestinal tract. While small quantities of yeast (reported as none or rare) may be normal, yeast observed in higher amounts (few, moderate to many) is considered abnormal.
An overgrowth of intestinal yeast is prohibited by beneficial flora, intestinal immune defense (secretory IgA), and intestinal pH. Beneficial bacteria, such as Lactobacillus colonise in the intestines and create an environment unsuitable for yeast by producing acids, such as lactic acid, which lowers intestinal pH. Also, lactobacillus is capable of releasing antagonistic substances such as hydrogen peroxide, lactocidin, lactobacillin, and acidolin.
Many factors can lead to an overgrowth of yeast including frequent use of antibiotics (leading to insufficient beneficial bacteria), synthetic corticosteroids, oral contraceptives, and diets high in sugar. Although there is a wide range of symptoms which can result from intestinal yeast overgrowth, some of the most common include brain fog, fatigue, recurring vaginal or bladder infections, sensitivity to smells (perfumes, chemicals, environment), mood swings/depression, sugar and carbohydrate cravings, gas/bloating, and constipation or loose stools.
A positive yeast culture (mycology) and sensitivity to prescriptive and natural agents is helpful in determining which anti-fungal agents to use as part of a therapeutic treatment plan for chronic colonic yeast. However, yeast are colonizers and do not appear to be dispersed uniformly throughout the stool.
Yeast may therefore be observed microscopically, but not grow out on culture even when collected from the same bowel movement.
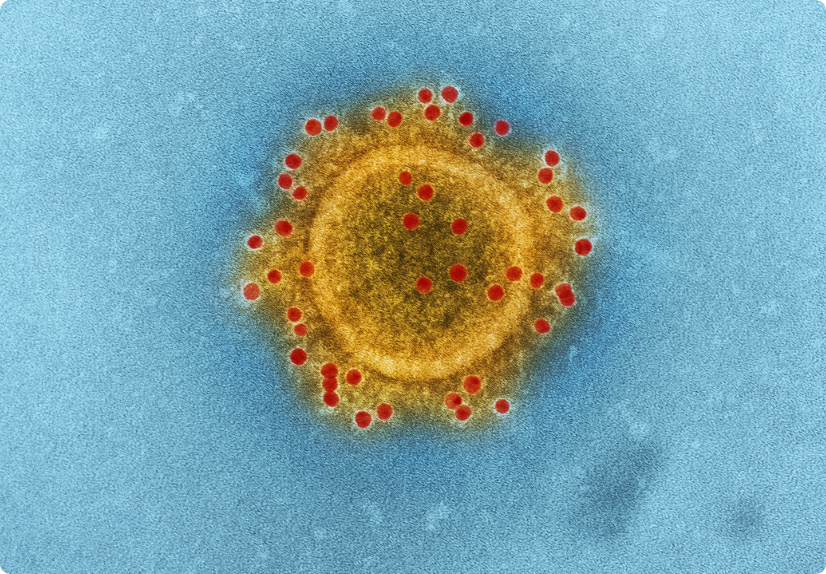
Intestinal parasites are abnormal inhabitants of the GI tract that live off and have the potential to cause damage to their host. Factors such as contaminated food and water supplies, day care centers, increased international travel, pets, carriers such as mosquitoes and fleas, and sexual transmission have contributed to an increased prevalence of intestinal parasites.
Parasites often have complex life cycles and routes of transmission. During this process parasites can be found as either TROPHS (active organisms) or CYSTS (dormant eggs or ‘ova’).
Note: Most parasites are acquired in their cyst state (before decystation within the body).
In general, acute manifestations of parasitic infection may involve diarrhoea with or without mucus and/or blood, fever, nausea, or abdominal pain. However, these symptoms do not always occur. Consequently, parasitic infections may not be diagnosed and eradicated. If left untreated, chronic parasitic infections can cause damage to the intestinal lining and can be an unsuspected cause of illness and fatigue. Chronic parasitic infections can also be associated with increased intestinal permeability, irritable bowel syndrome, irregular bowel movements, malabsorption, gastritis or indigestion, skin disorders, joint pain, allergic reactions, decreased immune function, and fatigue.
Blastocystis hominis is a common protozoan found throughout the world. Blastocystis is transmitted via the faecal- oral route or from contaminated food or water.
Whether Blastocystis infection can cause symptoms is still considered controversial. Symptoms may be compounded by concomitant infection with other parasitic organisms, bacteria, or viruses. Often, B. hominis is found along with other such organisms. Nausea, diarrhoea, abdominal pain, anal itching, weight loss, and excess gas have been reported in some persons with Blastocystis infection.
Medically recommended therapy can also eliminate G. lamblia, E. histolytica and D. fragilis, all of which may be concomitant undetected pathogens and part of patient symptomatology. Various herbs may also be effective. It is advisable to limit refined carbohydrates in diet.
Giardiasis is a diarrhoeal illness caused by the parasite Giardia intestinalis (also known as Giardia lambli). Giardia lamblia is flagellated protozoan that infects the small intestine and is passed in stool and spread by the faecal-oral route. Waterborne transmission is the major source of giardiasis.
Giardiasis is one of the most common parasitic infections in the western world, infecting nearly 2% of adults and 6% to 8% of children.
People become infected with Giardia by swallowing Giardia cysts found in contaminated food or water. Cysts are instantly infectious once they leave the host through faeces. An infected person might shed 1-10 billion cysts daily in their faeces and this might last for several months. However, swallowing as few as 10 cysts might cause someone to become ill. Giardia may be passed person-to-person or even animal-to-person. Also, oral-anal contact during sex has been known to cause infection. Symptoms of Giardiasis normally begin 1 to 3 weeks after a person has been infected.
Water filtration/sanitation is the primary method for reducing Giardia infection in the home, as well as maintaining good faecal hygiene practices around pets and bathroom.
Cryptosporidiosis is a diarrhoeal disease caused by an intestinal infection of Cryptosporidium parvum, a microscopic parasite. Cryptosporidiosis occurs worldwide and appears to be a relatively common cause of acute diarrhoea in young children, especially during warmer months of the year.
Cryptosporidium can spread from direct person-person contact or waterborne transmission. As well as infecting humans, Cryptosporidium parvum occurs in a variety of animals including dogs and cats. The infection is usually not serious in those with competent immune systems. However in situations of weakened immunity (e.g. cancer treatment, steroid therapy and HIV/AIDS) severe and long lasting illness may develop, and can be fatal.
The most common symptom is diarrhoea, which is usually watery and may be profuse. Other symptoms that may occur are nausea, vomiting, fever, headache and loss of appetite. However some infected with Cryptosporidium may appear asymptomatic.
Certain organisms release LPS when destroyed so detoxification support recommended – move slowly with any eradication protocols (which includes low carb diets) and monitor symptoms for progress.
Some pathogenic bacteria release cell fragments when destroyed that can trigger inflammatory and allergic responses – so supporting the immune system also recommended (anti-inflammatory and immune modulating agents most beneficial)
* NRF 2 is a powerful protein that lays dormant until turned on by an NRF 2 activator. Once released it migrates into the cell nucleus and binds to DNA at the location of ARE (Antioxidant Response Element) the master regulator of the entire antioxidant system present in every cell.
Sulforaphane Glucosinolate (SGS)
a natural substance from the seeds and sprouts of select broccoli varietals that, when ingested, begins breaking down in the gut (via healthy gut bacteria) to release sulforaphane, thereby up-regulating of the body’s own natural phase II detoxification enzymes.
SGS acts as an indirect antioxidant that provides long-lasting cell protection from free radical damage for days after being consumed by up-regulating endogenous celluar defence mechanisms.
A quality Elemental/Protein formula, Cod liver oil and Probiotic (that comply with the above) would provide the most succinct and yet comprehensive basis to any GIT/Immune support/treatment program.
FREE WEBINAR RECORDING
In this 2-part, 2 hour webinar, Dr Quig explains the many components of Doctor’s Data truly Comprehensive Stool Analysis, and provides a background on gastrointestinal research and how these advances have guided advances in functional testing technology and treatment.
Christina M Hester, Venkatakrishna R Jala, Morgan GI Langille, Shahid Umar, K Allen Greiner, Bodduluri Haribabu. Fecal microbes, short chain fatty acids, and colorectal cancer across racial/ethnic groups. World J Gastroenterol. 2015 Mar 7; 21(9): 2759–2769
Lagier et. al Microbial culturomics: paradigm shift in the human gut microbiome study. Clin Microbiol Infect. 2012 Dec;18(12):1185-93.
Tan KE, Ellis BC, Lee R, Stamper PD, Zhang SX, Carroll KC. Prospective evaluation of a matrix-assisted laser desorption ionization-time of flight mass spectrometry system in a hospital clinical microbiology laboratory for identification of bacteria and yeasts: a bench-by-bench study for assessing the impact on time to identification and cost-effectiveness. J Clin Microbiol. 2012 Oct;50(10):3301-8
Manz, Michael; Burri, Emanuel; Rothen, Claude; Tchanguizi, Nuschin; Niederberger, Christian et al. (2012) Value of fecal calprotectin in the evaluation of patients with abdominal discomfort: an observational study. BMC Gastroenterol. 2012 Jan 10;12:5.
Beilfuss HA, Quig D, Block MA, Schreckenberger PC. 2015. Definitive identification of Laribacter hongkongensis acquired in the United States. J Clin Microbiol 53:2385–2388.
While many labs have now adopted this technology, it’s important to note that not all MALDI-TOF is equal.
What to consider in the way of cause in the development of food sensitivity.
People tend to relate metabolism just with energy/weight, but it goes far beyond that.
Doctor’s Data, Inc. has provided innovative speciality testing to healthcare practitioners around the world from our advanced, CLIA-licensed clinical laboratory since 1972.
A specialist and pioneer in essential and toxic elemental testing, the laboratory provides a wide array of functional testing to aid in decision-making and better patient outcomes. Choose DDI to help you assess and treat heavy metal burden, nutritional deficiencies, gastrointestinal function, cardiovascular risk, liver and metabolic abnormalities, and more.

It is important to be informed as to where tests are being conducted as well as the technology used, so that you can be confident that your patients are performing evidence-based tests. RN Labs has always insisted in choosing laboratories that are of the highest standard globally with evidence-based functional tests, thereby improving patient outcomes and supporting the industry as a whole. RN Labs believes in maintaining full transparency of who and where your test is being carried out, so that you can make fully informed decisions with your patients.
We work with healthcare clinicians to bring their patient’s personalised care that’s unique to them.
We believe that every one of us is an individual when it comes to our health.
RN Labs Pty Ltd
18/93 Rivergate Place,
Murarrie, QLD 4172

Jess is a qualified Nutritionist with a Bachelor of Health Science in Nutritional Medicine. She believes that there is no one size fits all approach and is passionate about educating, inspiring and supporting clients and practitioners with a customised approach to healthcare. Specialties include preconception, pregnancy, post-natal and infant care.
Jess is excited to build relationships, educate and share her knowledge with both retail and practitioners in South Queensland and Northern NSW.

Lauren is an NHAA accredited Clinical Naturopath with a Bachelor of Health Science. She is incredibly passionate about natural health and educating clients on the foundational importance of nutrition, lifestyle and stress management and believes complimenting these building blocks with nutraceutical support and functional testing often holds the key to optimal health and vitality. Lauren looks forward to supporting practitioners and clients in these key areas.
Specialties include supporting thyroid health, digestive disorders and mental health.